Insurance Type Code is required for non-Primary Medicare payer. Element SBR05 is missing. It is required when SBR01 is not 'P' and payer is Medicare
Rejection MessageInsurance Type Code is required for non-Primary Medicare payer. Element SBR05 is missing. It is required when SBR01 is not 'P' and payer is Medicare. |
|
Rejection DetailsThis rejection occurs when Medicare is the secondary insurance and the Insurance Type code is missing. The Insurance Type indicates why the insured has Medicare as a secondary payer and is required when submitting secondary claims to Medicare. |
|
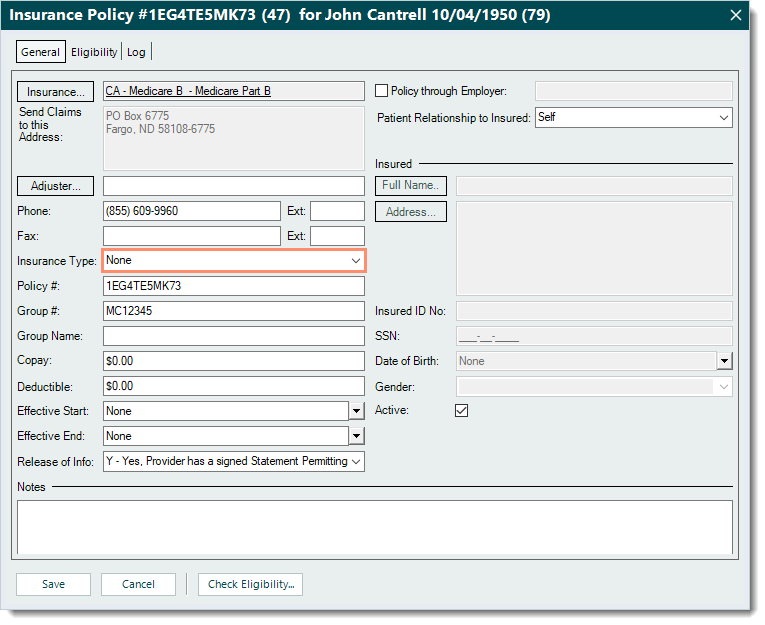
ResolutionFollow the steps below to enter the Insurance Type code:
Then, rebill and resubmit all affected claims when ready. |
 |