Contracts and Fees
Healthcare providers keep track of the procedures they perform, and associated fees for those procedures, through fee schedules. Fee schedules can be divided into two different categories: Standard Fees and Contract Rates.
Standard fee schedules and contract rates help you increase your collections by setting the right fees for your services and managing contracts to verify you're getting paid what you're owed from insurance companies. By closely managing your fees and contracts, you can increase your collections and eliminate manual audits.
Standard FeesThe standard fees are typically the default charges for the practice. Select the most common procedures and other services provided by the practice from the master list of CPT/HCPCS codes database and then enter fees to charge patients and out-of-network payers. Fees can be set for a specific combination of procedure and modifier. The fee schedule can be set for a specific provider and location or multiple providers and locations with an effective date range for which it applies. Get started and add a new standard fee schedule. |
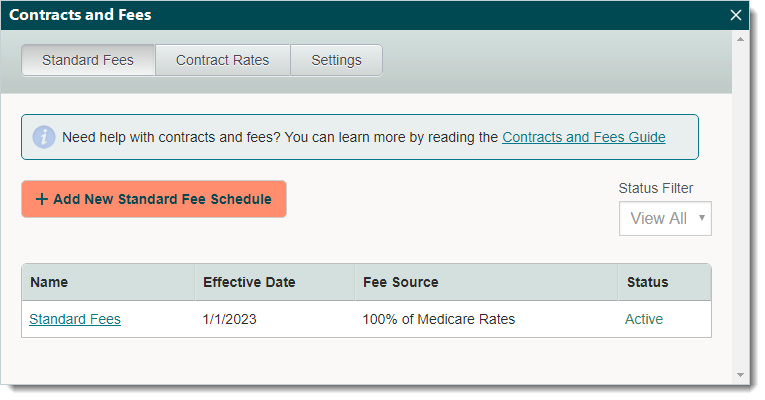 |
Contract RatesThe contract rates are pre-negotiated fees agreed upon between the provider and payer to join the payer's network. In addition to setting fees for each procedure, allowable amounts that correspond with the pre-negotiated fees can also be set. The contracts can apply to a specific provider and location or multiple providers and locations with an effective date range for which it applies. Set contractual response times required for paper and electronic claims (e-claims) to enable the Desktop Application (PM) to automatically flag claims if a response has not been received from the payer within the contractually required response time. Get started and add new contract rates. |
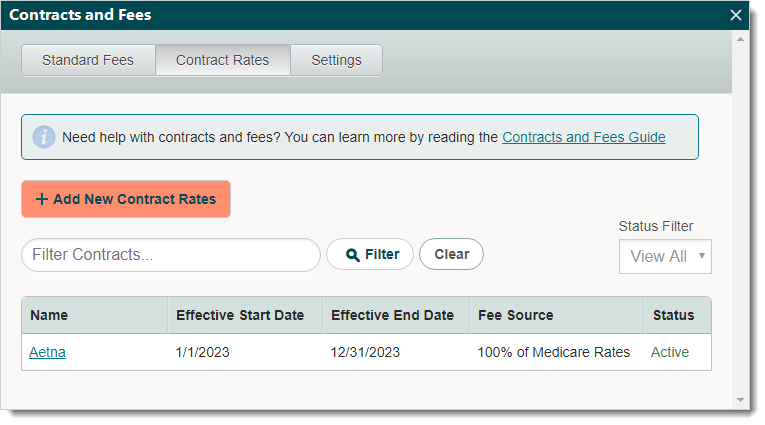 |
