OTHER PAYER CLAIM LEVEL ADJUSTMENT IS MISSING OR INVALID
|
Rejection Message OTHER PAYER CLAIM LEVEL ADJUSTMENT IS MISSING OR INVALID |
|
|
Rejection Details This rejection indicates that the adjudication information is missing on the claim from the primary payer. |
|
|
Resolution Verify that the payment from the primary insurance payment has been posted. |
|
|
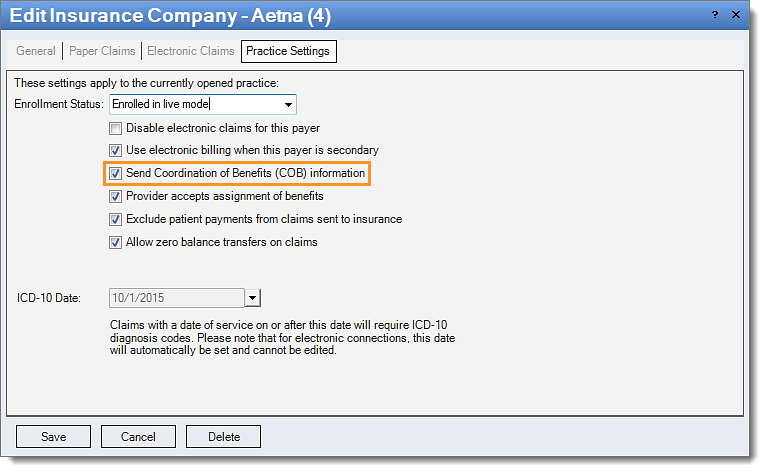
Follow the instructions below to verify that the primary payment is set up to send the payment information once the payment has been posted:
Then, rebill and resubmit all affected claims. |
 |