Other Payer Claim Filing Indicator Code is Invalid. Cannot = Medicare
|
Rejection Message Other Payer Claim Filing Indicator Code is Invalid. Cannot = Medicare |
|
|
Rejection Details This rejection indicates that the Insurance Program Type for both insurances billed on the claim was “Medicare.” When Medicare is listed as one of the payers on a claim, the other payer(s) listed cannot also have an Insurance Program of "MB- Medicare Part B." |
|
|
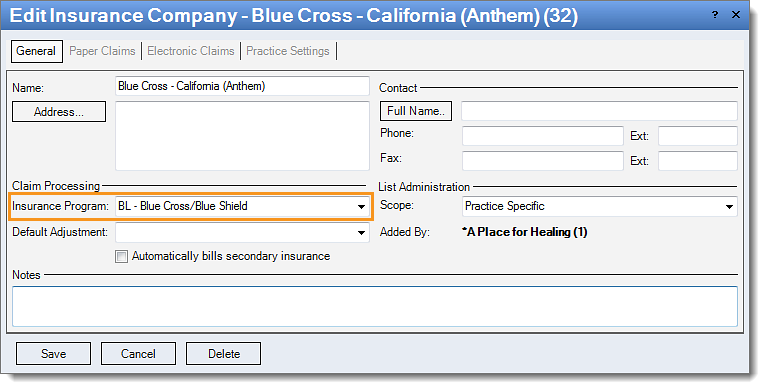
Resolution Follow the instructions below to change the insurance program code:
Then, rebill and resubmit all affected claims. |
 |