Subscriber and Other Subscriber Claim Filing Indicator Codes cannot both be MB
|
Rejection Message Subscriber and Other Subscriber Claim Filing Indicator Codes cannot both be MB |
|
|
Rejection Details Both insurances billed on the claim were Medicare. When Medicare is listed as one of the payers on a claim, the other payer(s) listed cannot also have an Insurance Program of MB- Medicare Part B. |
|
|
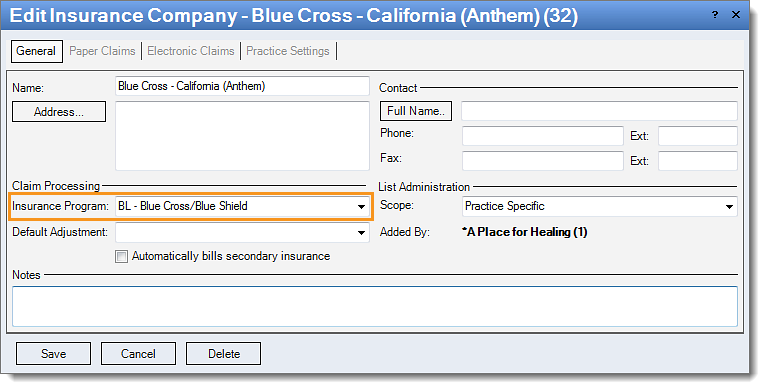
Resolution Follow these instructions to change the insurance program:
Then, rebill and resubmit all affected claims. |
 |