Electronic Claim Processing and Rejections
As part of claim processing, claims go through three separate reviews before reaching a payer’s internal adjudication system. You may receive electronic claim rejections from one or more of these reviewers: Kareo, the clearinghouse or the payer.
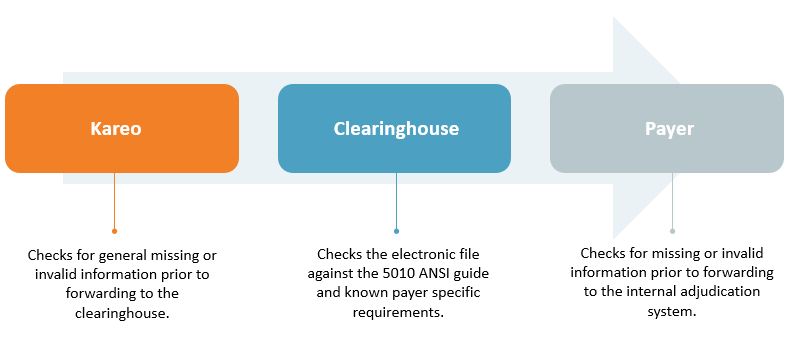 |
These reviews check for correct claim formatting rules (e.g., patient address, service location, diagnosis/procedure codes, payer ID). If there is missing or invalid information, the claim is prevented from being forwarded on to the next reviewer. When this occurs, a rejection report is generated for review to make the necessary correction(s) in order to resubmit the claim.
Claims rejected within Kareo are not forwarded to the clearinghouse. Timely filing cannot be generated for that submission until validation errors are corrected and the claim(s) resubmitted.
Once the claim passes through all three reviews for correct information, the claim goes on to the payer’s adjudication system. The payer then reviews the claim based on the patient’s insurance plan coverage and the contract with the provider; any claim denials at this stage are reported via an Electronic Remittance Advice (or paper remittance advice). To learn how to post claim denials, review Post and View Denied Claims.
