Clearinghouse Report Rejections
- Last updated
-
-
Save as PDF
Updated: 12/18/2025 | Views: 29198
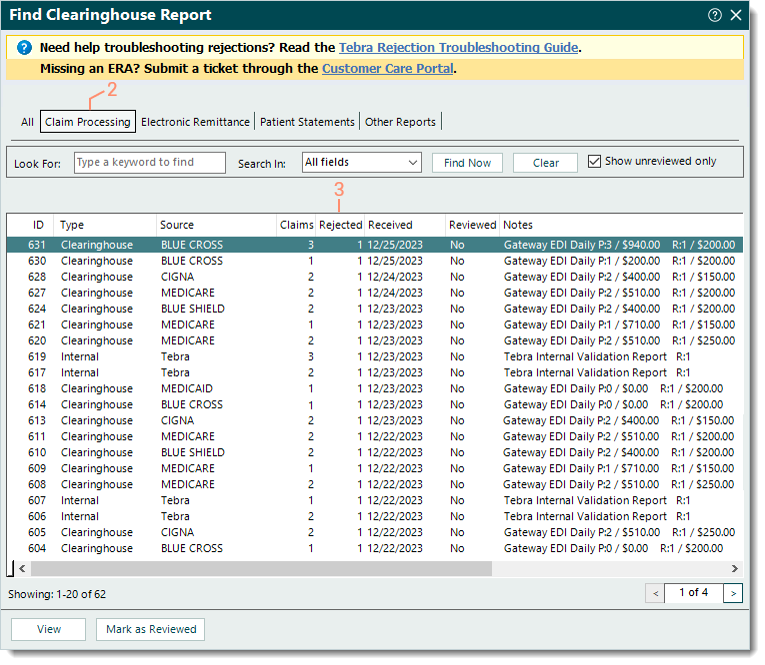
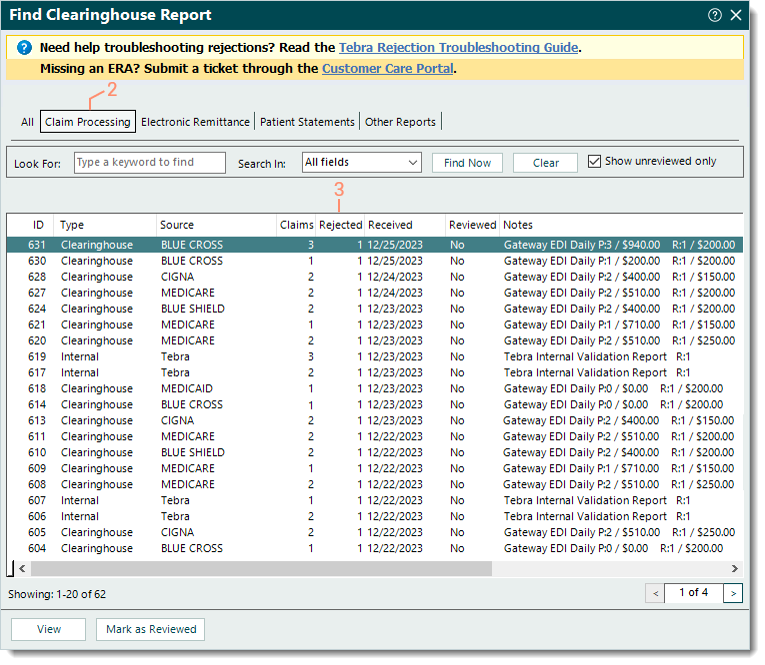
After submitting electronic claims (e-claims), claim processing reports are routed to the practice(s) within your Tebra account and can be found in the Clearinghouse Reports under the Claim Processing tab. You can access the Claim Processing reports list and view report details to identify rejections and next steps. The Claim Processing reports list includes Tebra internal validation reports, the clearinghouse acknowledgement/rejection reports, and the payer acknowledgement/rejection reports. It is recommended to monitor reports and take action on a daily basis.
Clearinghouse Report Rejections
- Click Encounters > Clearinghouse Reports. The Find Clearinghouse Report window opens.
- Click the Claim Processing tab. The Claim Processing reports list displays.
- Identify reports that include Rejected claims. Then, double click the report to open. The View Clearinghouse Report window opens.
- Review the report details of the:
- Make the appropriate corrections to resolve the claim rejection(s).
Note: Depending on the rejection, corrections may need to be made in the encounter, claim, practice and/or provider information and settings. To find a help article related to a specific rejection, search Claim Rejections.
- Once all corrective actions are complete, rebill and resubmit all affected claims when ready.
|
 |