Enable or Disable Psychotherapy Notes
Psychotherapy notes, also called process notes, are personal notes of a mental health care provider that are separate from the patient’s medical record and are not accessible by the patient, other providers, or staff members in the practice.
Psychotherapy notes are automatically enabled for mental health providers to create a new psychotherapy note from the patient's Notes page or through a clinical note. If the psychotherapy notes option is disabled, mental health providers can turn on psychotherapy notes for their own personal use. Or, providers can disable psychotherapy notes to remove psychotherapy notes option from the patient's chart and note.
Note: The psychotherapy note settings is set at the provider level. Changes made to these settings only affects the provider who is logged in and will not affect other providers in the practice.
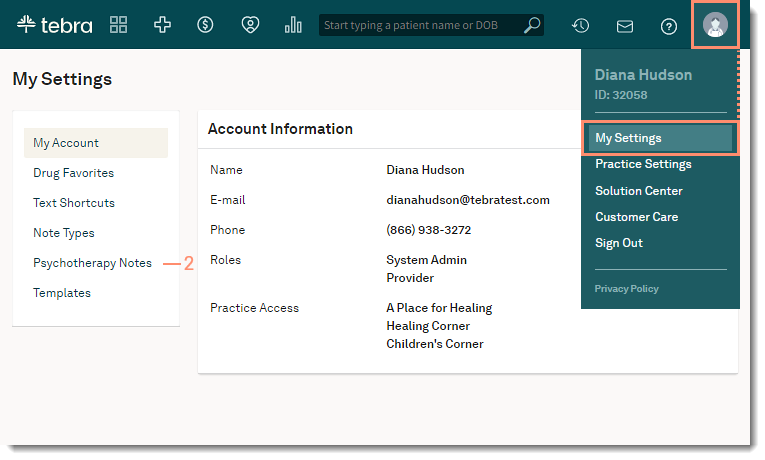
Access Psychotherapy Notes
|
 |
Enable Psychotherapy NotesPsychotherapy notes are automatically enabled for mental health providers. If the option is disabled, mental health providers providers can turn on psychotherapy notes for their own personal use.
|
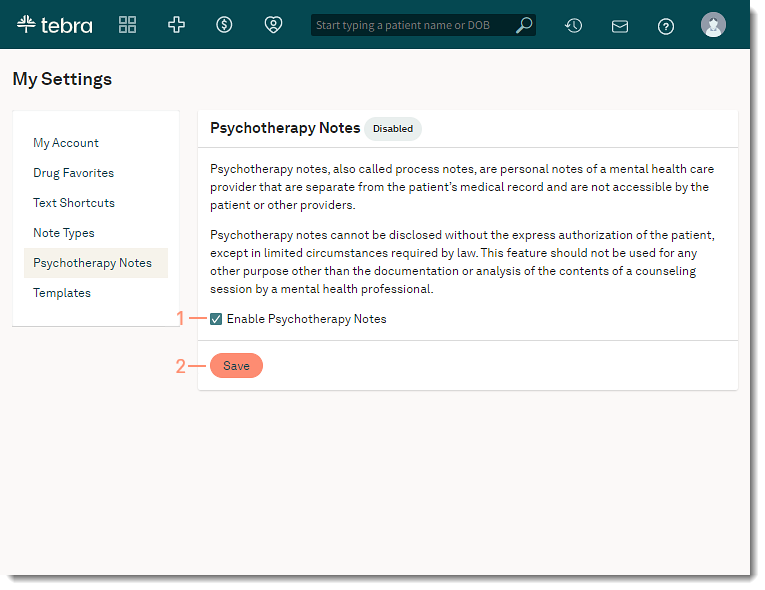 |
Disable Psychotherapy NotesProviders can disable psychotherapy notes to remove the psychotherapy note option from the patient's chart and note. Disabling this option will not delete existing psychotherapy notes. Providers can enable the option again to restore access to the existing psychotherapy notes. If applicable, delete the patients psychotherapy notes to permanently delete all documentation before disabling the option.
|
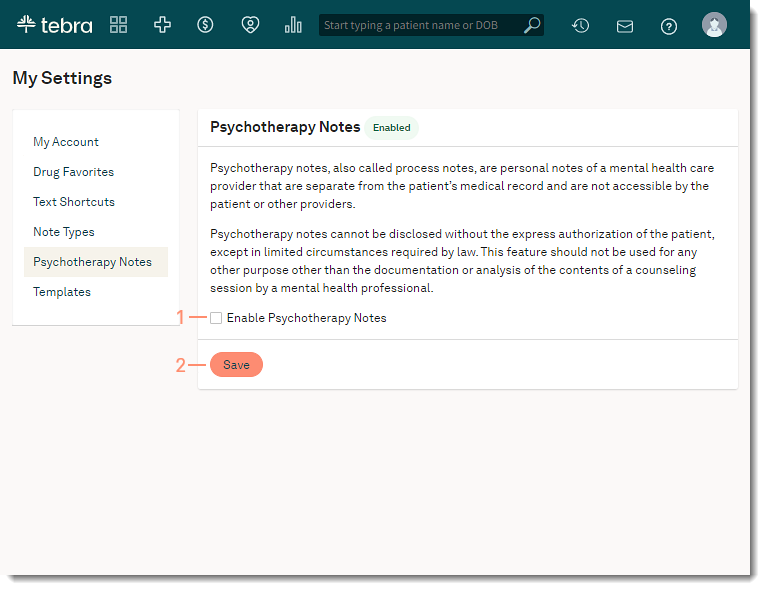 |
