Create Psychotherapy Note
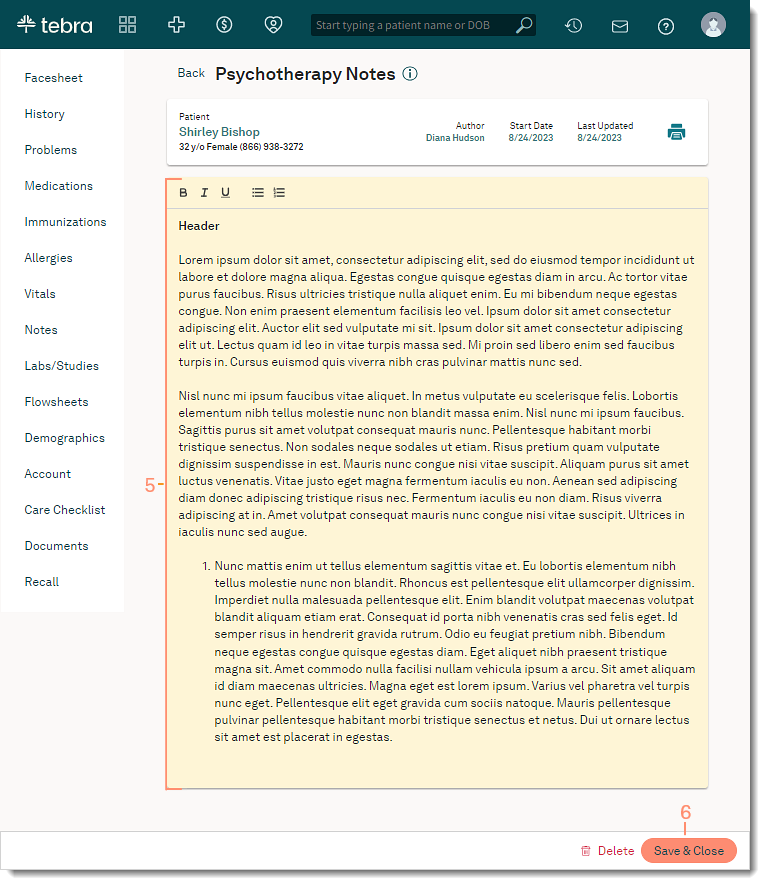
Psychotherapy notes, also called process notes, are personal notes of a mental health care provider that are separate from the patient’s medical record and are not accessible by the patient, other providers, or staff members in the practice.
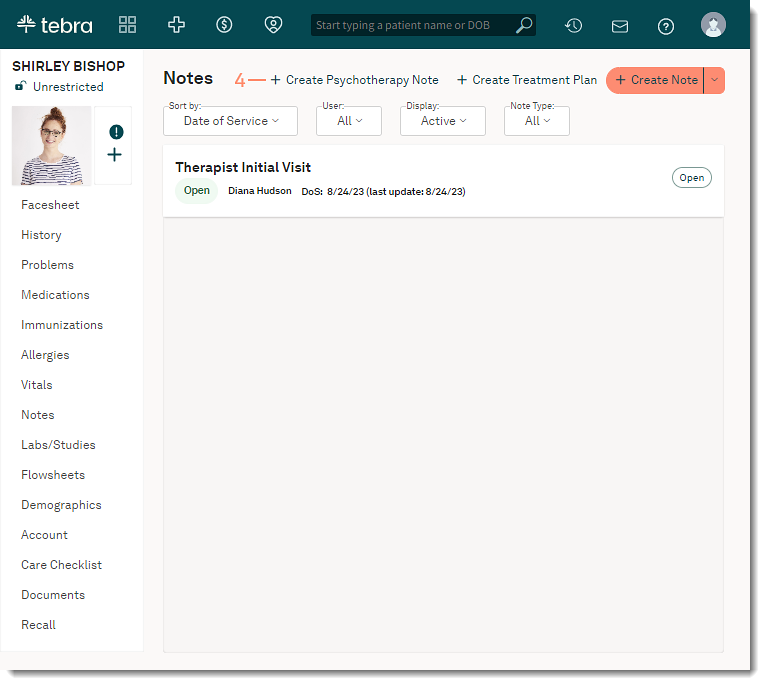
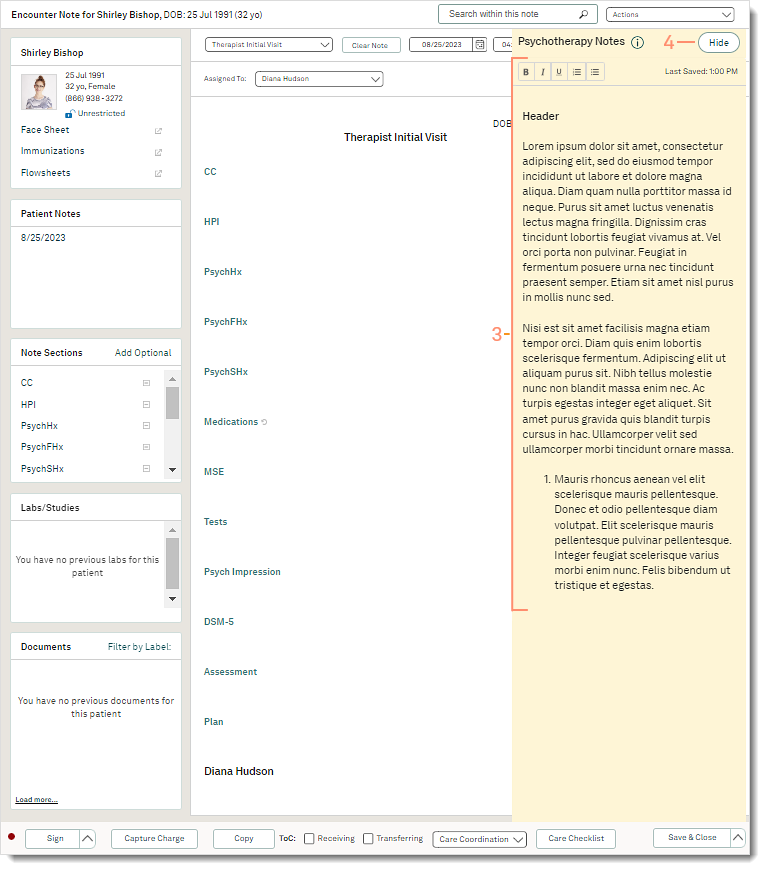
Psychotherapy notes are automatically enabled for mental health providers. Providers can create psychotherapy notes to document their personal observations and insights related to the therapeutic session from the patient's Notes page or through a clinical note. Only one psychotherapy note can be created for the patient per provider. Providers can also view or edit the psychotherapy note in a clinical note. This allows providers to enter their clinical documentation and access their personal notes at the same time.
The psychotherapy note is separate from the medical chart and is not included in any Health Information Exchange (HIE) such as referrals, patient chart printouts, clinical note printouts, patient portal, and CCDA. Psychotherapy notes cannot be disclosed without the express authorization of the patient, except in limited circumstances required by law. This feature should not be used for any purpose other than the documentation or analysis of the contents of a counseling session by a mental health professional.
The psychotherapy note is automatically saved approximately every 30 seconds or when a change is made to the note to increase productivity and avoid data loss.
Create from Notes Page
|
 |
|
 |
|
 |
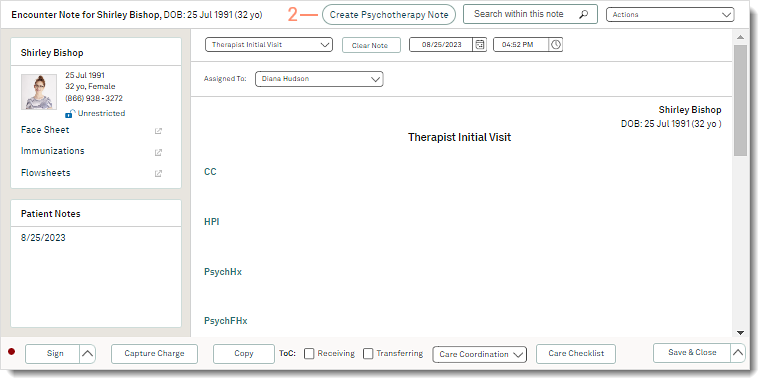
Create from Clinical NoteCreate, view, or edit the psychotherapy note in a clinical note. Providers can enter their clinical documentation and access their personal notes at the same time.
|
 |
|
 |
