Edit or Delete Psychotherapy Note
Psychotherapy notes, also called process notes, are personal notes of a mental health care provider that are separate from the patient’s medical record and are not accessible by the patient, other providers, or staff members in the practice.
When psychotherapy notes are enabled, providers can create psychotherapy notes and continue editing to document their personal observations and insights related to the therapeutic session. The option to edit a psychotherapy note is available from the patient's Notes page or through a clinical note. If the psychotherapy note is no longer necessary in the patient's chart, the psychotherapy note can be permanently deleted.
Psychotherapy notes cannot be disclosed without the express authorization of the patient, except in limited circumstances required by law. This feature should not be used for any purpose other than the documentation or analysis of the contents of a counseling session by a mental health professional.
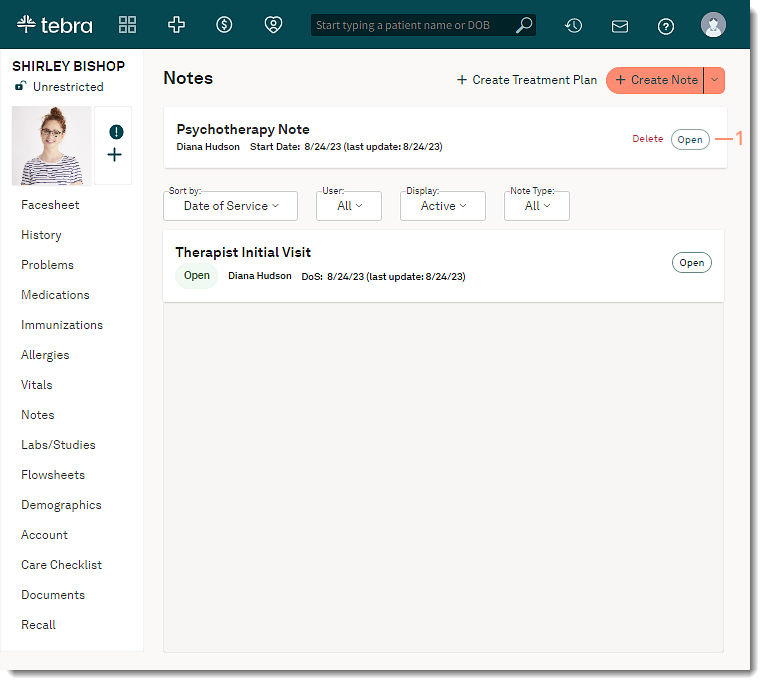
Access Patient Notes
|
 |
Edit Psychotherapy NoteThe option to edit a psychotherapy note is available from the patient's Notes page or through a clinical note. The provider can continue to document their personal notes in the patient's psychotherapy note. The psychotherapy note is automatically saved approximately every 30 seconds or when a change is made to the note to increase productivity and avoid data loss. Edit from Notes Page
|
 |
|
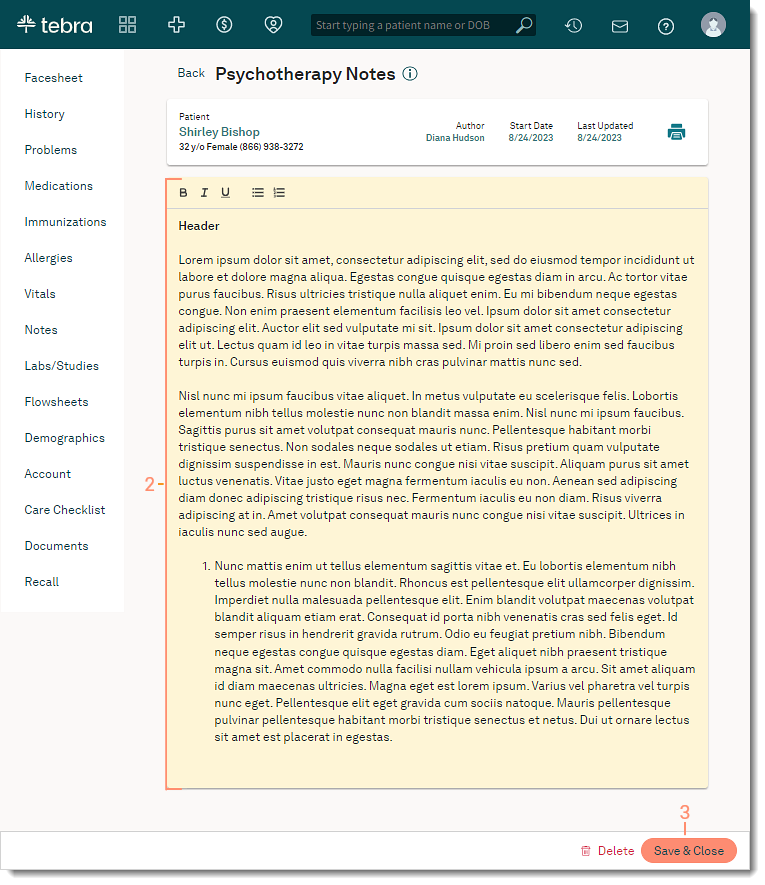 |
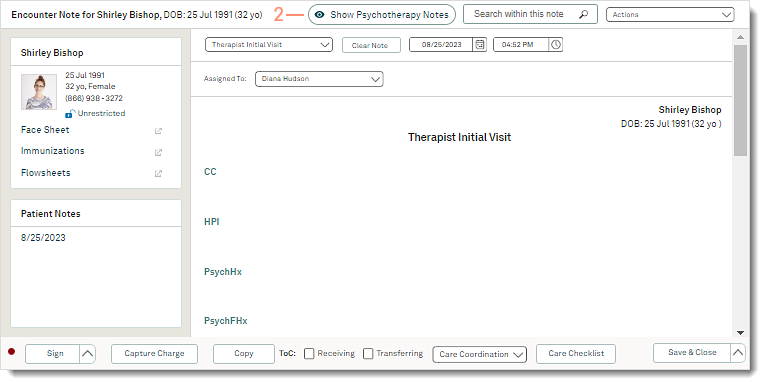
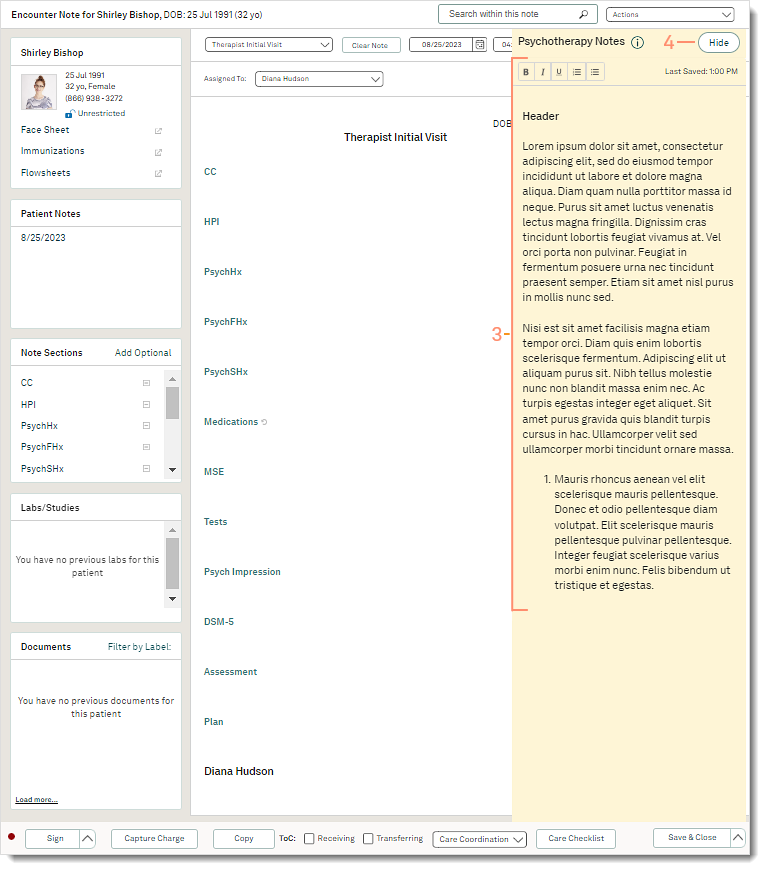
Edit from Clinical NoteProviders can enter their clinical documentation and edit their personal notes at the same time. The psychotherapy note is automatically saved approximately every 30 seconds or when a change is made to the note to increase productivity and avoid data loss.
|
 |
|
 |
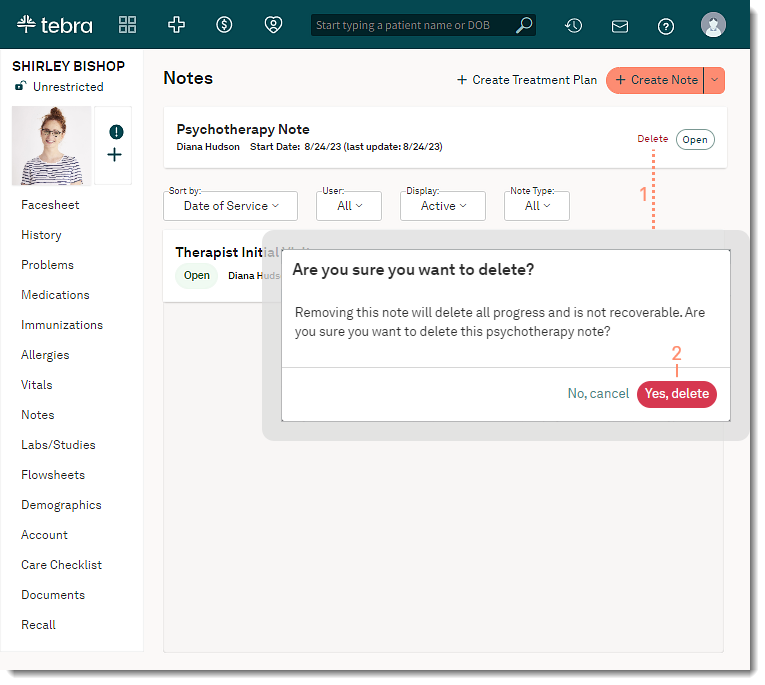
Delete Psychotherapy NoteThe psychotherapy note can be deleted if the psychotherapy note is no longer necessary in the patient's chart. Removing the note will permanently delete all documentation and is not recoverable.
|
 |
