Updated: 03/04/2020
Views: 6286
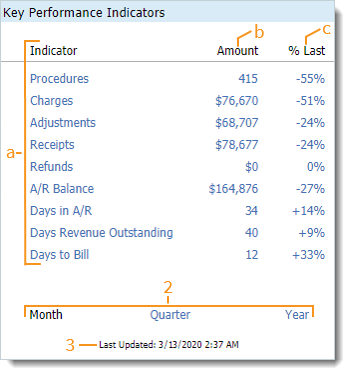
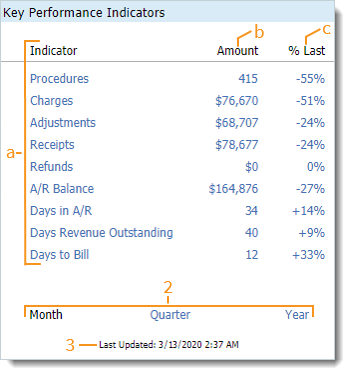
The Key Performance Indicators enable you to monitor the key metrics that impact the financial and operational health of the practice. To understand how key indicators are calculated, review Key Indicators Reports.
Key Performance Indicators
- The Key Performance Indicators table is comprised of the following.
Note: Click on any of the hyperlinks within the table to view the Key Indicators Summary report.
- Indicator: The name of the Key Performance Indicator.
- Procedures: Total procedures rendered to patients.
- Charges: Total charges billed to insurance and patients.
- Adjustments: Total adjustments made to charges.
- Receipts: Total amount collected.
- Refunds: Total amount of refunds issued.
- A/R Balance: Total amount in accounts receivable waiting for payment.
- Days in A/R: Average number of days that charges are in accounts receivable from the date of billing until the date of receipt of payment.
- Days Revenue Outstanding: Average number of days that charges are outstanding from the date of service until the date of receipt of payment.
- Days to Bill: Average number of days to bill an encounter.
- Amount: The metric associated with the Key Performance Indicator.
- % of Last: The percentage change between the last and the current accounting period.
- Accounting periods of activity include:
- Month: Selected by default and displays month-to-date metrics in the table.
- Quarter: Click to select and display quarter-to-date metrics in the table.
- Year: Click to select and display year-to-date metrics in the table.
- Last Updated: The date and time the Key Performance Indicators were last calculated automatically by the system.
|
 |