Updated: 07/28/2023 | Views: 7996
If a claim was rejected due the patient's eligibility, follow the instructions below to verify their eligibility and edit the Patient record as necessary. When all corrective actions are completed, rebill and resubmit all affected claims.
Verify Patient Eligibility
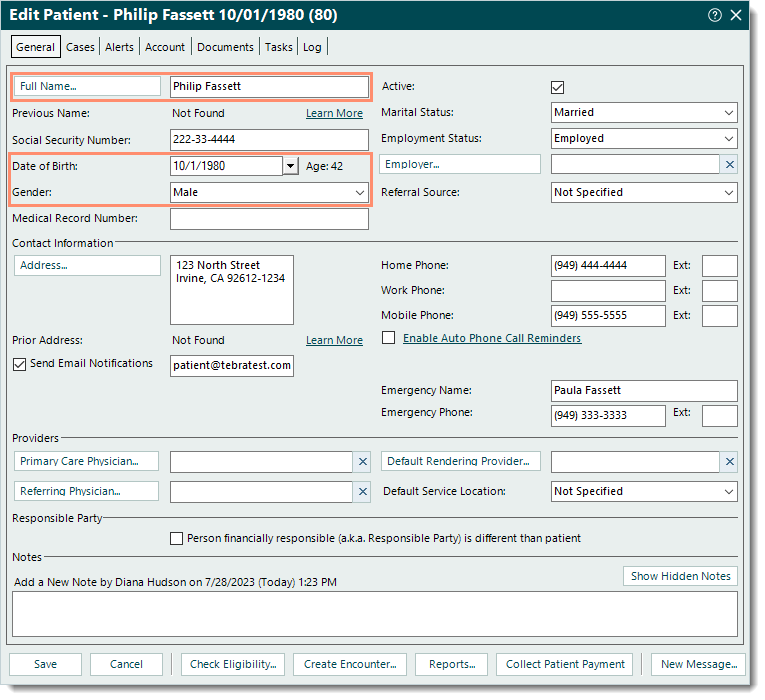
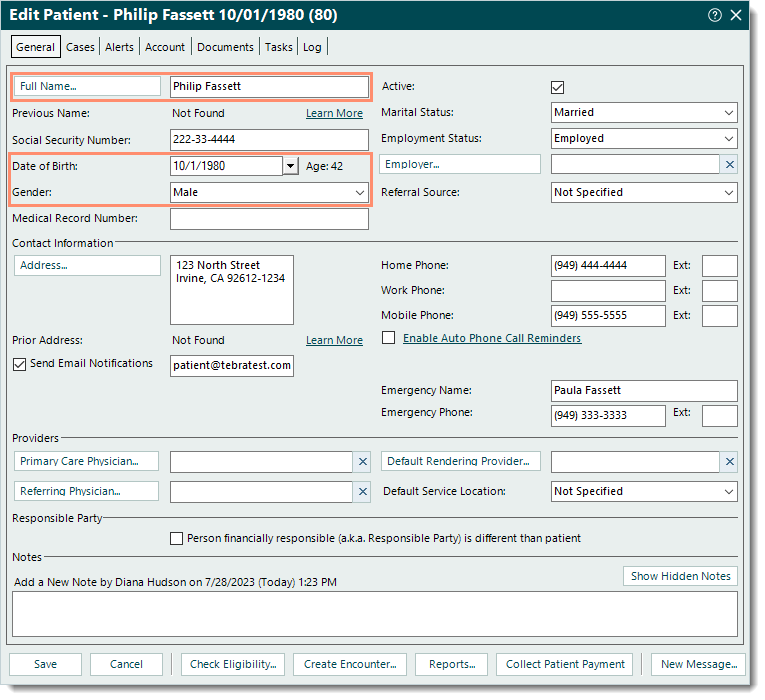
- Find the Patient record then double click to open it. The Edit Patient window opens.
- Verify the following information against the patient's insurance card and edit as necessary: Full Name, Date of Birth, and Gender.
|
 |
- Click the Cases tab then double click to open the appropriate case. The General tab of the Edit Case window opens.
- Under the Insurance section, double click the policy to open. The Insurance Policy window opens.
- Verify the following information as applicable and edit as necessary.
- Policy # and Group #.
- Patient Relationship to Insured, and Insured demographics.
- To save any corrections made, click Save at the bottom of each relevant window until it is no longer available.
|
 |
- Check patient eligibility for active coverage for the claim's date of service.
Note: The information that displays on Check Patient Eligibility window is based on the window it was opened from (e.g., Find Patient, Edit Patient, Insurance Policy).
- If patient eligibility check is not available or does not display active coverage, verify the patient's eligibility directly with the payer and notate the following information.
- Phone number for the payer
- Reference number for the call
- Name of the payer representative
If all patient demographics and eligibility are confirmed by the payer, contact Customer Care for further assistance.
Note: Tebra's clearinghouse partners require a copy of the patient's insurance card (front and back) in order to research eligibility rejections. Have a copy available in the Patient record or ready to be provided to Customer Care via another secure method.
|
 |