Updated: 04/30/2025 | Views: 11714
You can manually apply zero payments received from insurance companies. This transfers the allowed balance amount(s) (e.g., applied to deductible, coinsurance) to the patient or secondary insurance for further billing, and is a necessary step if the secondary insurance claims are submitted electronically.
Apply Zero Payment
Follow the steps below to apply a $0.00 insurance payment due to the patient deductible and/or coinsurance. An example remittance advice (RA) is provided for reference.
|
Example Remittance Advice (RA):

|
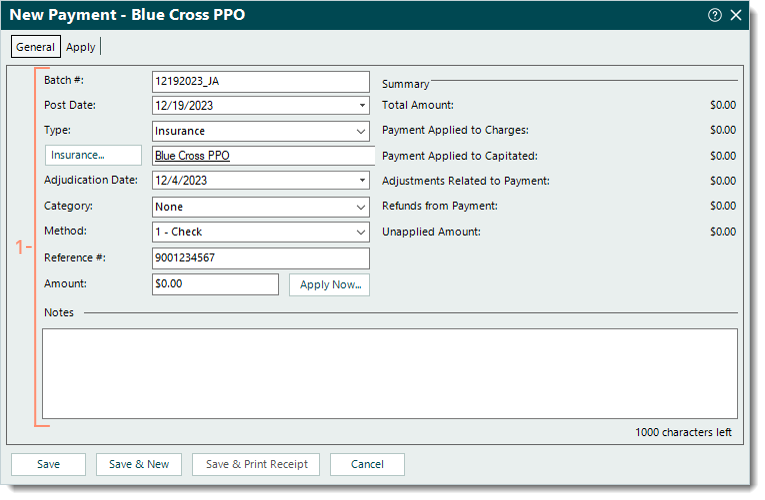
- Create a new insurance payment and enter the information as necessary under the General tab. Then, click Apply Now. The Apply tab opens.
|
 |
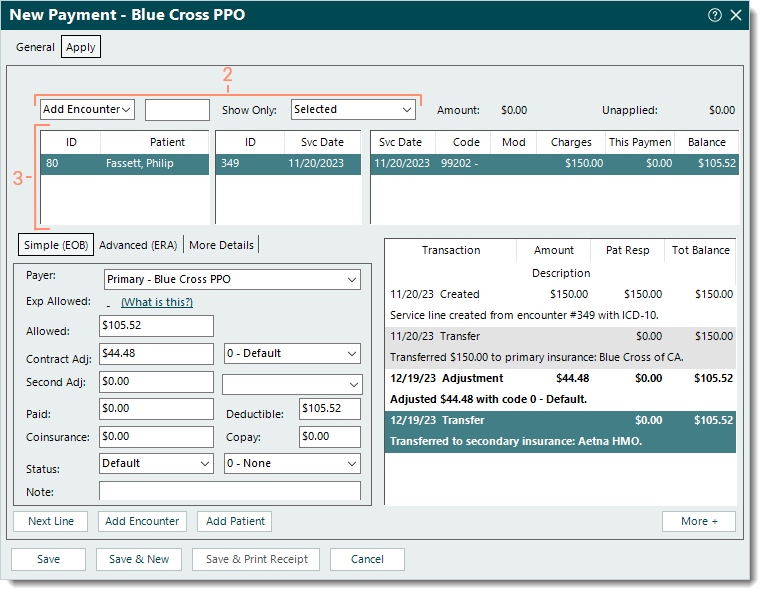
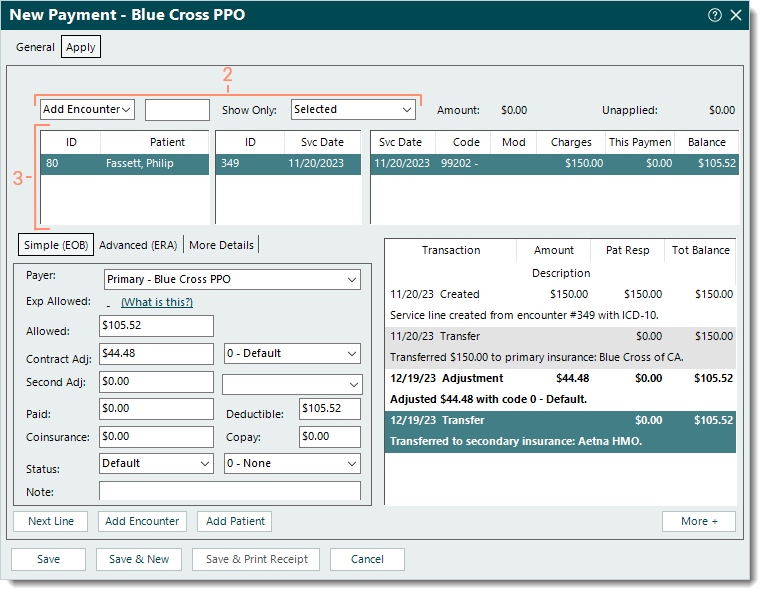
- Use the top options to add the encounter or patient as necessary.
- The first drop-down menu defaults to Add Encounter. To add service lines by patient ID instead, click the drop-down arrow and select Add Patient.
Note: When an encounter is added, all service lines associated with the encounter are listed. When a patient is added, all open service lines associated with the patient are listed.
- In the open text field, enter the encounter ID, patient's name, or patient ID. Then, press Enter on the keyboard. The service lines are listed.
Note: The encounter ID may be indicated as the Patient Account Number or Claim Reference ID on the RA as follows: Encounter ID + Z + Tebra Account ID (e.g., 176Z15050).
 Tip: To limit results and avoid having to search and select the Encounter record, enter the encounter ID + Z (e.g., 176Z) to quickly add the encounter. Tip: To limit results and avoid having to search and select the Encounter record, enter the encounter ID + Z (e.g., 176Z) to quickly add the encounter.
- If the Select Encounter or Find Patient window opens, search and select the record.
- Show Only: Defaults to Selected. Click the drop-down arrow to select a different option.
- Click once to select the patient, encounter, and/or service line the zero payment amount needs to be applied to.
|
 |
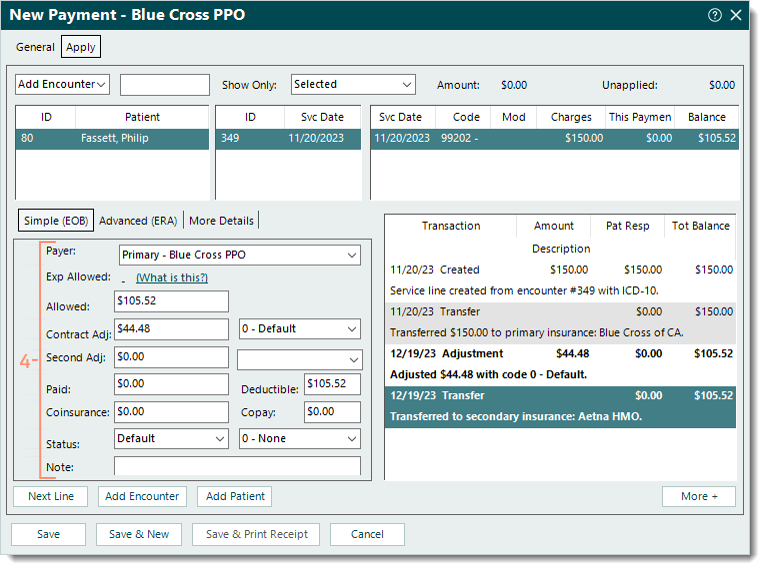
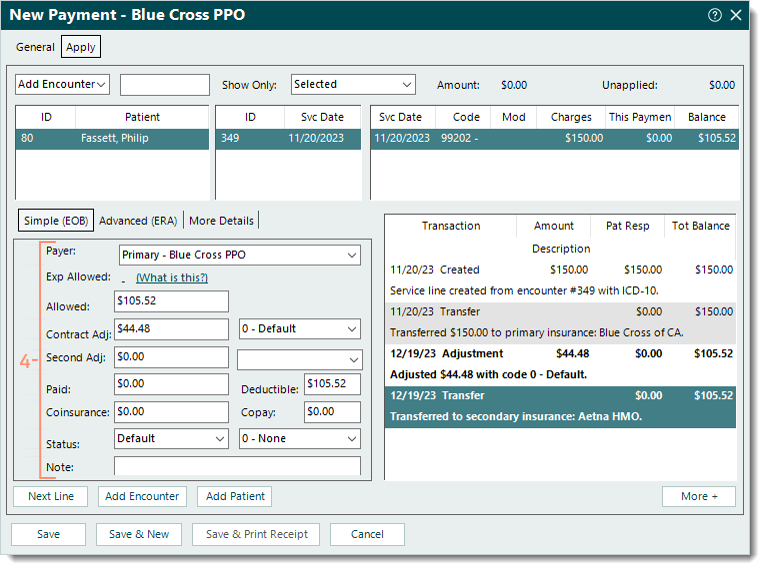
- Under the Simple (EOB) tab, enter the following information.
Note: As the information is entered, verify the transaction lines (in bold) posted on the right side of the window are correct. Once the payment is saved, these transaction lines are posted under the Transactions section of the corresponding Claim record.
- Payer: The payer auto-populates from the Insurance selected on the General tab of the payment.
- Allowed: The reported allowed amount (e.g., $105.52).
- Contract Adj: Automatically calculated when using Tab on the keyboard to advance to the next field (e.g., $44.48). If necessary, enter the amount. Then, select the appropriate adjustment code from the drop-down menu.
Note: The codes available for selection pull from the Adjustment Codes list. If a Default Adjustment is entered on the Insurance Company General Settings for the payer, that adjustment code auto-populates.
- Second Adj: The reported second adjustment amount and adjustment code if applicable.
- Paid: Leave as $0.00.
- Deductible: The reported deductible amount if applicable (e.g., $105.52).
- Coinsurance: The reported coinsurance amount if applicable.
- Copay: The reported copay amount if applicable.
- Status: If necessary, select a specific status update from the drop-down menu. Then, select a reason code from the drop-down menu if applicable.
Note: The last transaction line should indicate the balance is transferred to the secondary payer if the patient has a secondary insurance policy. If not, select Bill payer 2. Then, select a reason code from the drop-down menu if applicable.
- Note: Internal notes related to the zero payment that will display when viewing transaction line details.
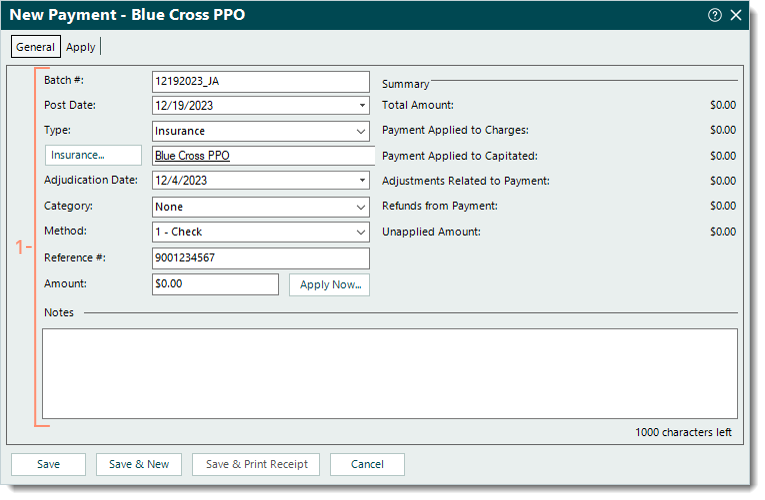
- Once finished with the selected service line, continue as necessary.
- To continue applying zero payment amounts, click Next Line if it should be applied to the next service line listed, or click to select the appropriate service line. Then, repeat steps 4-5 as necessary.
- To return to the top options and add another encounter or patient, click Add Encounter or Add Patient. Then, repeat steps 2-5 as necessary.
- If finished applying the zero payment(s) to the corresponding service line(s), click Save. If a confirmation pop-up appears, click Yes to post the payment with a $0.00 amount.
Note: For a zero payment reported on a paper RA, it is recommended to open the Payment record and upload the RA under the Documents tab. Refer to the Tebra account agreement details and pricing policy for applicable document storage fees.
Then, submit the claim to the secondary payer or send a patient statement for the balance when ready.
|
 |