Apply Payment from Paper Remittance Advice (RA)
- Last updated
-
-
Save as PDF
Updated: 01/08/2026 | Views: 28585
Once the General tab information for a payment from the insurance company is entered the appropriate amounts of the payment are manually applied to the corresponding service lines as reported on a paper provider remittance advice (e.g., explanation of payment, standard paper remittance), or the patient explanation of benefits (EOB).
Manually Apply Payment from Paper Remittance Advice (RA)
- Find the payment then double click to open. The General tab of the Edit Payment window opens.
- Click Apply Now. The Apply tab opens.
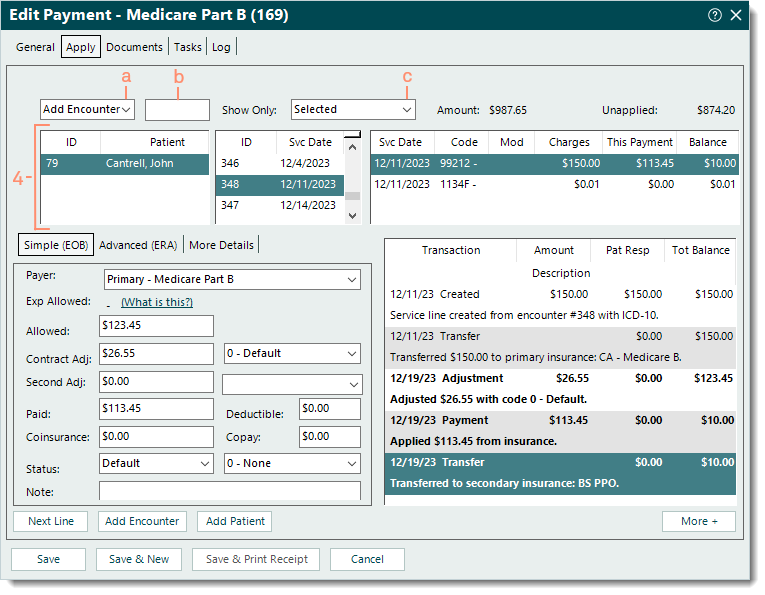
- Use the top options to add a patient or encounter as necessary.
- The first drop-down menu defaults to Add Encounter. To add service lines by patient ID instead, click the drop-down arrow and select Add Patient.
Note: When an encounter is added, all service lines associated with the encounter are listed. When a patient is added, all open service lines associated with the patient are listed.
- In the open text field, enter the encounter ID, patient's name, or patient ID. Then, press Enter on the keyboard. The service lines are listed.
Note: The encounter ID may be indicated as the Patient Account Number or Claim Reference ID on the paper RA as follows: Encounter ID + Z + Tebra Account ID (e.g., 176Z15050).
 Tip: To limit results and avoid having to search and select the Encounter record, enter the encounter ID + Z (e.g., 176Z) to quickly add the encounter. Tip: To limit results and avoid having to search and select the Encounter record, enter the encounter ID + Z (e.g., 176Z) to quickly add the encounter.
- If the Select Encounter or Find Patient window opens, search and select the record.
- Show Only: Defaults to Selected. Click the drop-down arrow to select a different option.
- Click once to select the patient, encounter, and/or service line the payment amount needs to be applied to.
|
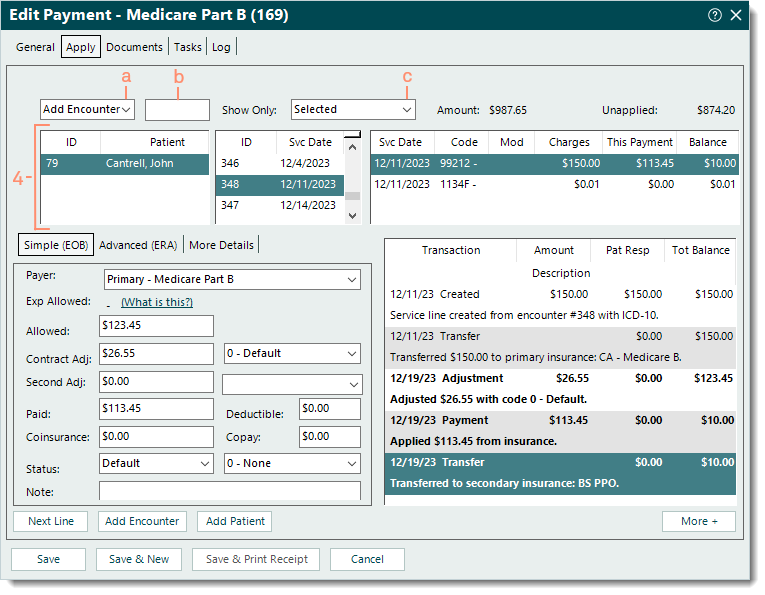 |
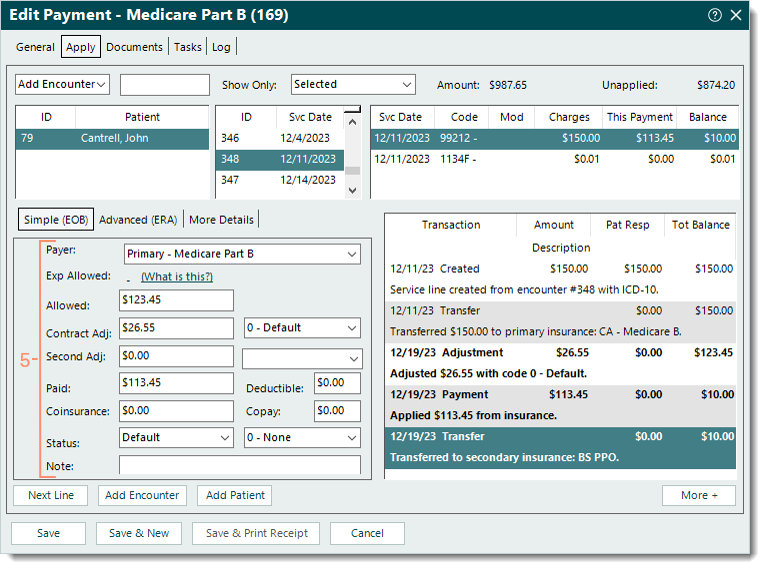
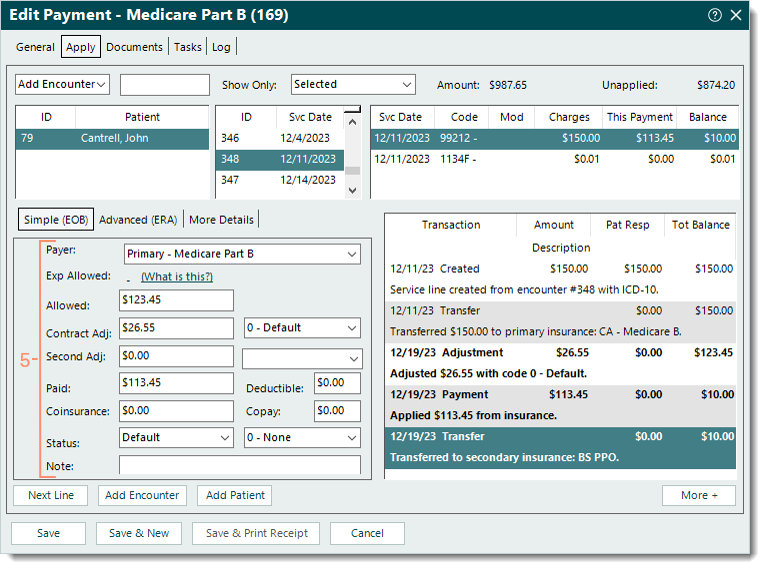
- Under the Simple (EOB) tab, enter the following information.
Note: As the information is entered, verify the transaction lines (in bold) posted on the right side of the window are correct. Once the payment is saved, these transaction lines are posted under the Transactions section of the corresponding Claim record.
 Tips for primary insurance payments: The sum of the Allowed, Contract Adj, and Secondary Adj amounts should equal the charge amount. The sum of the Paid, Deductible, Coinsurance, and Copay amounts should equal the Allowed amount. Tips for primary insurance payments: The sum of the Allowed, Contract Adj, and Secondary Adj amounts should equal the charge amount. The sum of the Paid, Deductible, Coinsurance, and Copay amounts should equal the Allowed amount.
- Payer: The payer auto-populates from the Insurance selected on the General tab of the payment.
- Allowed: The reported allowed amount. If the claim was denied, leave as $0.00.
- Contract Adj: Automatically calculated when using Tab on the keyboard to advance to the next field. If necessary, enter the amount. Then, select the appropriate adjustment code from the drop-down menu
Note: The codes available for selection pull from the Adjustment Codes list. If a Default Adjustment is entered on the Insurance Company General Settings for the payer, that adjustment code auto-populates.
- Second Adj: The reported second adjustment amount and adjustment code if applicable.
- Paid: The amount of the payment to apply to the selected service line.
- Deductible: The reported deductible amount if applicable.
- Coinsurance: The reported coinsurance amount if applicable.
- Copay: The reported copay amount if applicable.
- Status: If there is a remaining balance after the payment amount is applied, select the appropriate status update from the drop-down menu. Then, select a reason code from the drop-down menu if applicable.
- Note: Internal notes related to the payment amount applied that will display when viewing transaction line details.
- Once finished with the selected service line, continue as necessary.
- To continue applying amounts of the payment, click Next Line if the amount should be applied to the next service line listed, or click to select the appropriate service line. Then, repeat steps 5-6 as necessary.
- To return to the top options and add another encounter or patient, click Add Encounter or Add Patient. Then, repeat steps 3-6 as necessary.
- If finished applying all amounts of the payment to the corresponding service line(s), verify the Unapplied amount displays $0.00 then click Save.
Note: Once saved, it is recommended to open the Payment record and upload the paper RA under the Documents tab. Refer to the Tebra account agreement details and pricing policy for applicable document storage fees.
 Tip: To view a report of how the payment was allocated, open the Payment record, click Reports on the bottom of the Edit Payment window and select Payments Application. Tip: To view a report of how the payment was allocated, open the Payment record, click Reports on the bottom of the Edit Payment window and select Payments Application.
|
 |